What is Arthritis?Arthritis in a joint occurs when the gristle on the ends of the bone wear out so that bones are touching. This situation usually occurs as a gradual process as the gristle or articular cartilage gradually thins as the cartilage degenerates.
What does arthritis feel like?
Arthritis causes pain (usually a dull ache), swelling, loss of movement and altered shape of the knee (deformity). The loss of function maybe represented by difficulties in stair climbing, walking and standing.
If the arthritis affects the knee cap (patellofemoral joint) the pain tends to occur on bent knee activities such as stair climbing and walking on inclines or slopes.
If the arthritis affects the weightbearing (femorotibial) part of the joint then standing and walking on the flat produce the most symptoms.
How is the Diagnosis Made?
Standing Xrays of the knee and special views of the kneecap will usually confirm the diagnosis. Early degrees of degeneration leading to arthritis can usually be detected by MRI scans.
What treatments are available?
Simple treatments include pain killers (paracetamol is the safest), anti-inflammatory tablets and creams. It is very important to maintain a normal body weight and a gentle exercise program to maintain movement and muscle tone. Physiotherapy will help with setting out a suitable exercise program. Knee supports or braces maybe useful in some cases. Injections of Cortisone maybe helpful. Hyalagan injections have not been found to be particularly useful.
 Surgical Treatments
Surgical Treatments
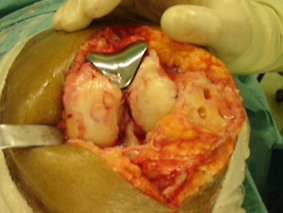
Joint replacement is the mainstay of surgical treatment for the established arthritic knee. This is usually discussed after non operative treatments have been tried.
Joint replacement includes Total Knee Replacement (TKR), part or Unicompartment Replacement (usually on the inner side of the knee), and a patello femoral replacement.
The outcome studies for TKR are published and established with 95% of knee replacements lasting for 10-15 years. Unicompartmental replacements have a similar outcome and patellofemoral replacements have good outcomes but the information is limited as it is a less commonly used operation.
Unicompartmental and patellofemoral replacement do have certain advantages over TKR in terms of speed of recovery and range of movement but each person needs to be assessed individualy regarding suitability for this surgery.
 Other developments such as Minimal Incision (invasive) Surgery and Computer Navigated Surgery may have advantages, but the available literature does not indicate any significant improvement at this stage. Long term studies are required. The concerns are the longer anaesthetic times and the ability to perform an adequate operation through a limited access.
Other developments such as Minimal Incision (invasive) Surgery and Computer Navigated Surgery may have advantages, but the available literature does not indicate any significant improvement at this stage. Long term studies are required. The concerns are the longer anaesthetic times and the ability to perform an adequate operation through a limited access.
The publicity regarding "Spacers" which are metal discs inserted into the arthritic joint needs to be approached with caution. This technique was used before many years ago and was unsuccessful. This technique needs to have proper medical literature review.
Arthrodesis or fusion of the knee maybe considered for young patients with an arthritic knee, but is a very uncommon operation in orthopaedic practice.
In early or localised osteoarthritis, Osteotomy (High Tibial Osteotomy HTO) operations to straighten the leg have a place especially in young people under 50. This maybe combined with cartilage or meniscal transplantation. Each person needs to be assessed individualy regarding suitability for this surgery. The rehabilitation maybe quite prolonged and therefore close liaison with the physiotherapist will be required.

Patellofemoral Arthritis
Who gets it?
This condition tends to occur in people in their forties or above, it is more common in women, particularly if overweight and it maybe hereditary. Previous dislocations of the patella may cause arthritis and the condition commonly affects both knees.
What does patellofemoral arthritis feel like?
The problems are the same as for anterior knee pain, although people may complain of more of a background ache at the front or back of the knee. The pains are usually more constant and the knee may be more inclined to swell. The knees tend to be more noisy and creaky especially on stairs.
How is the diagnosis made?
The diagnosis is confirmed by examination. X rays may also confirm the diagnosis although in early disease X rays maybe normal but an MRI scan maybe useful in identifying the early changes.
What treatments are available?
Initial treatment includes pain killers and anti inflammatories, weight reduction and an exercise program (physiotherapy) .
Weight reduction is vital because stair climbing puts 6-7 times our body weight through the knee cap so loss of a stone reduces the force through the knee by 6-7 stone. This alone may be enough to alleviate symptoms.
Again the use of knee supports and shoe insoles maybe helpful.
Surgical treatment includes keyhole surgery and release of the kneecap. The kneecap tends to become tighter as it becomes arthritic the soft tissues on the outer side of the knee tighten pulling the kneecap to the outer side of the knee. Releasing the knee cap (lateral release) may help to reduce pain. Smoothing the back of the kneecap (chondroplasty) is usually undertaken at the same time.
The pressure behind the kneecap can also be relieved by moving the attachment of the patella tendon to the shin bone or tibia, this is called a tibial tubercle transfer (TTT). This is a more complex procedure with a longer recovery period but can be highly effective. These treatments may also be combined with treatments to repair the articular cartilage such as microfracture, chondrocyte implantation and osteochondral grafting.
In more severe cases where the gristle or articular cartilage is extremely worn, joint replacement of the patellofemoral joint maybe considered. Removal of the kneecap (patellectomy) maybe considered in rare cases but is generally avoided nowadays.
The kneecap joint makes up one of the three compartments of the knee joint and when the knee joint is affected by arthritis it usually affects the inner side compartment of the joint (medial) and the kneecap compartment.
The outer side or lateral compartment of the knee joint is much less commonly affected by arthritis, but when this is the case the kneecap joint is nearly always affected. The kneecap maybe affected in isolation in 15% of people with osteoarthritis of the knee joint.



Back to top